The Direct Payments (PB/PHB) Practioner Guide to Better Decisions
My recent blog that
explored the need to have proper conversations on direct payments,https://haloabletec.blogspot.com/2021/12/direct-payments-including-health.html got a lot of hits. Obviously, this is a topic
of interest, so I have given it a bit more thought to see what I, as a practitioner,
would do in your shoes. If I was a member of a CCG/Team or Adult Social Care Team,
how would I decide if what was asked for is appropriate? This is not a legal opinion;
these are merely suggestions that may help me weigh up the decisions in
your roles.
As I said in my previous post, I understand the pressures on staff via the government
to reduce expenditure in our public services. Unless a major change happens in
people's views this is not going to change. The main parties all want to reduce
expenditure. This really doesn't help staff in these roles as the legislation
for personalisation giving independence, choice and control, including the
NHS Constitutional right to patients’ choice, and the Care Act all give people
these legal rights. My personal view is that legislation trumps austerity.
There have been no legislative laws brought in with regard to austerity, it is
but a particular government’s wishes and views, however, I fully take on board
this doesn't help either.
In my view, there has to be a balance between needs beings met and what a
person thinks they are entitled to. For those in both Social Care and The NHS I
would suggest the starting point to be look at the “Principles of Wellbeing”
laid under section 1 of the Care Act. Yes, there is a legal definition for
wellbeing, not just made-up service or name for feeling ‘good’. The principles
give you an aim to work towards, as to how it benefits the person. The
statutory guidance under the care Act is where you'll find further information on
using wellbeing principles. They state that these should be used to justify or
give reasoning behind the assessment process in the Care Act. To date and
I've asked plenty of times, I've never seen an assessment done with these principles.
The New white paper on Social Care highlights that the Act is a good price of
legislation it just isn't used how it's supposed to be and this point is one of
the very ones the Government are making.ie the need to make decisions based on
effects to life.
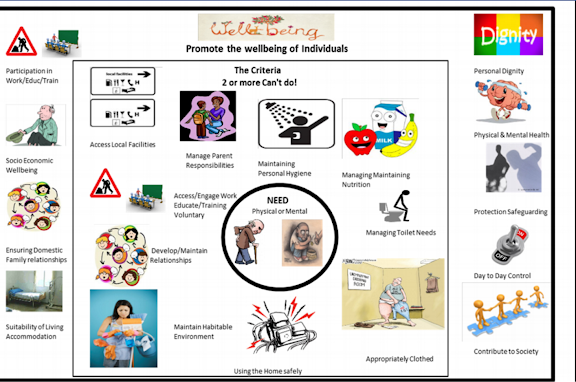
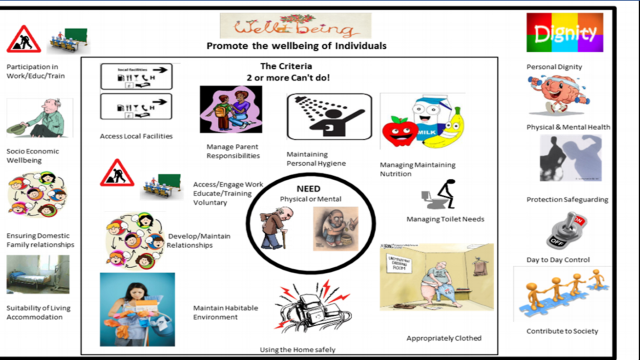
Below are two pictures I’ve created and used to help me and others understand
the points above. The first is the explanation of needs under the Care Act and
the graphics in the middle box that are assessed and identified as "needs". The
outer box shows the wellbeing principles thus if a need is presented say the
need for maintaining personal hygiene, this could be shown as meeting the wellbeing principles
of Dignity.
The above is just a first step in how better decisions can and should be made (remember this is statutory guidance).
The other decisions that often concern practioner is the benefit factor I.e. what benefit does the person derive from the expenditure, or more unsaid, is it
likely that others might benefit too? To this I would add can the benefit be
made in alternative manner, which is cheaper and more cost effective? The
argument here being we can't all have what we want. It's got to be reasonable, whether
you have a budget or not, want isn’t need. The other reasoning is how often the
person is likely to benefit from it, and the additional costs involved
(electric, water). When it comes to both, preservation of life and safeguarding
must always be the main priority.
One of the questions that gets thrown around when discussing budgets is regarding public accountability. So why not ask yourself this question, not as a practitioner, not as a recipient, but would you, as a member of the public, think in this circumstance that this is fair? Again, this is a practical decision, over want and need.
These questions are not out of thin air, but via what I know about some of the things accepted as allowable in the early days of budgets. For example, where the overall principles of get what you can, often even I questioned against whether it was a necessary expenditure or the need could have been met better and cheaper by alternative means. Having been through a number of these assessments, both social care and CCG, as budget holder myself and in advocating for others, I have used the above process to both justify to practioner and challenge users whether their requests were justified.
I hope this blog makes people think and have better conversations, in the end
help both parties to come to a rational over the budget, and where independence,
choice and control is not lost, whilst ensuring a fair and equitable system for
direct payments can be retained.

This comment has been removed by the author.
ReplyDelete